what is facial nerve paralysis or facial palsy?
Habilitation therapy care focuses on improving the quality of life for individuals facing challenges such as paralisis facial or facial nerve paralysis. This type of care helps restore function and confidence in those affected by conditions like idiopathic facial nerve paralysis, often referred to as what is facial nerve palsy. By addressing the specific needs of patients, habilitation therapy incorporates strategies that support recovery, adapt to new limitations, and optimize facial muscle function. With a focus on patient-centered care, therapists work to ensure that individuals regain as much control as possible over their facial movements.
Facial paralysis, which occurs when the facial nerve is damaged, can result from infections, trauma, or unknown causes. In cases of idiopathic facial nerve paralysis, also called Bell’s palsy, symptoms often arise suddenly and can affect one or both sides of the face. This condition causes drooping, weakness, and a loss of muscle control, making simple tasks like smiling or closing an eye difficult. Effective management involves tailored therapies that may include exercises, massage, or medical interventions to encourage recovery. With the right care, even severe cases of facial nerve paralysis can show significant improvement over time.
Types of Facial Palsy
Facial palsy can be caused by a variety of factors, leading to different types based on the underlying cause. Bell’s palsy is one of the most common types, characterized by temporary paralysis on one side of the face, often linked to viral infections like the herpes simplex virus. It usually resolves on its own, but corticosteroids can help speed up the recovery process. Another type, congenital facial palsy, occurs from birth due to improper development of the facial nerve or associated structures, and it may be linked to syndromes such as Möbius syndrome.
Other forms of FP are linked to physical trauma or tumor-related causes. Traumatic facial palsy can occur from skull fractures, surgical complications, or blunt force injuries that damage the facial nerve. On the other hand, tumor-related FP happens when growths like acoustic neuromas or parotid gland tumors press on the nerve, causing weakness or paralysis. Infectious facial palsy results from diseases like Lyme disease or Ramsay Hunt syndrome, both of which can damage the facial nerve. Stroke-related facial palsy, which affects the brain’s ability to control facial movements, typically spares forehead movement and differs from peripheral causes like Bell’s palsy. Lastly, post-surgical facial palsy happens when the nerve is unintentionally damaged during surgeries on the ear, head, or neck.
- Bell’s palsy
- congenital facial palsy
- physical trauma or tumor-related
- Infectious facial palsy
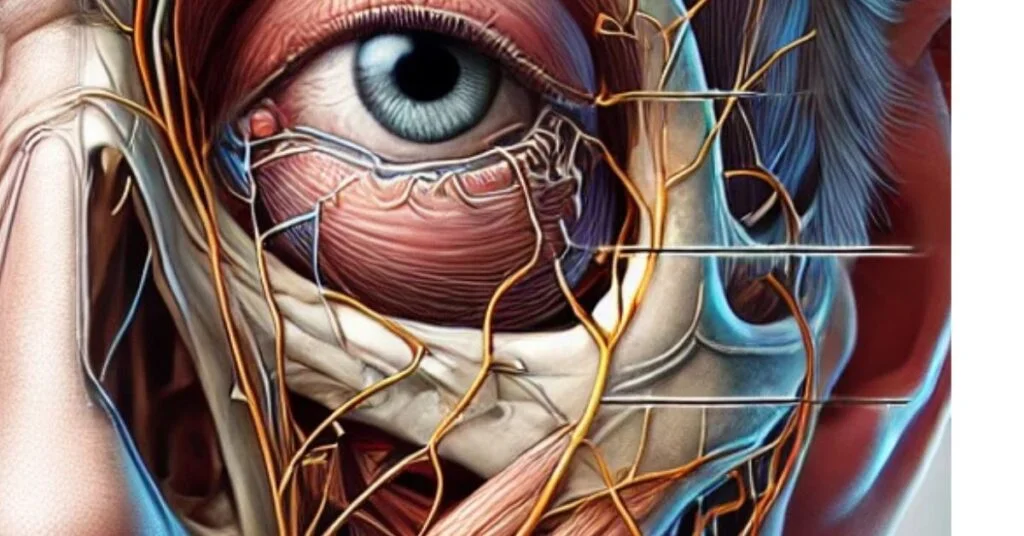
Facial nerve involvement and their possible complications after nerve paralysis
Facial nerve paralysis, also referred to as facial palsy, occurs when the facial nerve (cranial nerve VII) is damaged. This nerve controls most of the facial muscles and also plays a key role in functions like taste on the anterior two-thirds of the tongue, tear production, and saliva regulation. When the facial nerve becomes impaired, it can lead to facial asymmetry, drooping of the mouth, eye droop, and difficulty with facial expressions, such as smiling and blinking. The condition may affect one side of the face (unilateral) or both sides (bilateral), and the damage may vary in severity.
The complications of facial nerve paralysis are wide-ranging. Some individuals may experience incomplete recovery, leaving them with persistent weakness or abnormal recovery. Over time, synkinesis can develop, where involuntary movements occur, such as an attempt to smile causing the eyes to close. Additionally, muscle contractures can lead to tightness in the face and result in facial distortion, such as a pulled-down corner of the mouth. Dry eyes may occur due to the inability to blink, leading to irritation and potential corneal damage.
Other complications include loss of taste in the affected area of the tongue, hyperacusis (increased sensitivity to sound), and facial pain around the ear or along the facial nerve. If other nerves like the trigeminal nerve or vagus nerve are affected, patients may experience numbness, swallowing difficulties, or even voice changes. Early treatment and rehabilitation, including facial exercises and eye protection, are essential for minimizing these complications and promoting recovery.
What are the causes of facial palsy or paralysis?
Facial nerve paralysis can occur due to a variety of reasons, ranging from viral infections to physical trauma. One of the most well-known causes is Bell’s palsy, an acute facial nerve paralysis that often appears suddenly. The condition can be linked to herpes simplex infection, with symptoms developing over several days to months. Though the exact cause is not always clear, Bell’s palsy is typically clinically diagnosed and often recovers spontaneously. Treatment, such as corticosteroids, may help reduce symptoms.
Other causes include Lyme disease, which is transmitted by ticks carrying the Borrelia burgdorferi bacteria, and Ramsay Hunt syndrome, which is caused by the reactivation of the varicella-zoster virus. These conditions can lead to facial nerve damage and symptoms such as ear pain, vesicles, and sensorineural hearing loss. In some cases, tumors, such as acoustic neuromas or parotid gland neoplasms, can also compress the facial nerve, leading to facial paralysis. Additionally, head trauma, like blunt trauma or fractures to the skull, can cause direct damage to the facial nerve.
In more severe cases, surgical causes like the removal of a facial nerve tumor or issues arising from a middle ear infection can damage the nerve. Facial nerve compression from high pressure or tumors can also cause dysfunction, sometimes requiring decompression surgery. Treatment options vary, including nerve grafting, muscle transfer techniques, and surgical exploration, depending on the severity of the injury and the underlying cause.
Facial palsy or paralysis diagnostic tests
Diagnosing facial palsy begins with a detailed assessment of the patient’s symptoms, and medical history, and a neurological examination to pinpoint the exact cause of the paralysis. Observation of facial movements, such as the ability to smile, blink, or raise the eyebrows, is critical. A unique feature that aids diagnosis is whether the forehead wrinkles; its presence often suggests central facial palsy, while its absence points toward peripheral facial palsy. This distinction is crucial for identifying whether the cause is a UMN lesion, such as a stroke or subdural hematoma, or an LMN lesion, such as a viral infection like HSV-1, CMV, or EBV.
In cases where physical examination alone cannot identify the cause, additional tests are performed. A CT scan or MRI is vital for detecting tumors, temporal bone fractures, or intra-cranial or extra-cranial abnormalities. If there is a history of exposure to tick habitats during warmer months or signs like rash, headache, and fever, Lyme disease becomes a likely diagnosis. Here, a serological test confirms the FP. Similarly, if symptoms such as pain, blisters in the ear, and hearing issues occur, Ramsey Hunt’s syndrome may be suspected, requiring targeted antiviral treatment.
For conditions linked to infections, tests like blood tests or X-rays are useful. Complications from acute otitis media, cholesteatoma, or even parotid malignancy can be assessed through imaging or direct examination. Furthermore, classifying the paralysis into supranuclear lesions, involving areas like the pontine arteries or facial nucleus, or intranuclear lesions helps narrow down the diagnosis. The time course of symptoms, whether acute, subacute, or chronic, also provides insight into the underlying pathology.
Effective diagnosis requires combining clinical skills with modern imaging and laboratory tools to accurately identify the root cause of facial palsy. This ensures that treatment can be tailored to the individual’s condition.
Treatments that are best for facial palsy or paralysis
The treatment of FP relies on its causes. For example, if the condition arises from a stroke, the focus will be on managing the stroke itself. In cases of tumors, doctors may opt to surgically remove them to alleviate pressure on the facial nerve. When it comes to facial nerve palsy treatment caused by Bell’s palsy, healthcare providers often prescribe corticosteroids early on to reduce inflammation and swelling in the facial nerve.
Nonsurgical options such as physical therapy help improve facial symmetry, boost muscle strength, and restore facial coordination. Speech therapy is another key approach to improving communication and swallowing functions. For some individuals, Botox injections can address involuntary movements like synkinesis, while occupational therapy can assist with enhancing everyday interactions.
In severe cases where recovery is incomplete, surgical options like reanimation surgery can restore movement. This often involves nerve transfers, muscle transplants, or tendon transfers to regain lost function. Cosmetic procedures such as brow lifts or facelifts can also enhance appearance and bring back balance to the face.
Proper eye care is vital, especially when blinking is disrupted. Treatments include artificial tears, lubricating drops, and sometimes eyelid surgery to protect the eyes from becoming too dry. Each case is unique, so personalized approaches are essential for effective results.
What people want to know
What is the main cause of facial palsy?
The primary cause of facial palsy varies, but Bell’s palsy, an acute condition often linked to herpes simplex virus, is the most common. Other causes include Lyme disease, Ramsay Hunt syndrome, tumors like acoustic neuromas, and trauma to the facial nerve. Infections, strokes, or surgical complications can also lead to facial palsy.
How to treat facial paralysis at home?
Home care for facial paralysis includes: Facial exercises to improve muscle strength. Gentle massage to stimulate circulation.Protecting the eye with artificial tears, ointments, or patches if blinking is impaired.Eating soft foods to avoid strain on facial muscles.
What is the major difference between BP and FP?
Facial palsy is a broad term for any paralysis caused by facial nerve dysfunction. Bell’s palsy is a specific type of facial palsy with no identifiable cause other than suspected viral inflammation.